Survey done by Lucknow University students on tobacco control issues in Lucknow
Acknowledgement: -
We express our sincere gratitude to Professor Dr Rama Kant, Head, Department of General Surgery, Chhatrapati Shahu Ji Maharaj Medical University (CSMMU, upgraded King George's Medical College - KGMC) and Chairman, Tobacco Cessation Clinic at CSMMU supported by World Health Organization (WHO), for his extensive invaluable guidance to make our internship an enormous learning experience. We are also thankful to Mr Abhishek Misra and Mr Ritesh Arya who gave their precious time for data collection. We feel short of words to thank the young legendary tobacco control advocate, public health crusader and prolific writer Mr Amit Dwivedi for his unflinching support, guidance and mentorship. We are also thankful to all the 763 respondents who have given their precious time to talk to us and make this effort successful.
Background
Tobacco is the most preventable cause of death in the world today. This year, tobacco is estimated to kill more than five million people – more than tuberculosis, HIV/AIDS and malaria combined. By 2030, the death toll due to this deadly substance is likely to exceed eight millions a year. Unless urgent action is taken, tobacco could kill one billion people during this century. Although tobacco deaths rarely make headlines, tobacco kills one person every six seconds.
Policies
In India, tobacco kills more than one million (10 lakhs) people annually. To control tobacco usage and reduce the occurrence of life-threatening diseases, disabilities and deaths caused by tobacco use, the Government of India brought into effect one of the most comprehensive tobacco control policy – The Cigarette and Other Tobacco Products Act 2003. Since then, different rulings and processes have been giving shape to enforce the various provisions of this Act. India has also signed ( and the Indian parliament has ratified) the first global corporate accountability and public health tobacco treaty – the Framework Convention on Tobacco Control (FCTC) on 5 th February 2005. Despite existing tobacco control policies, not only the number of juvenile and young tobacco users continues to rise unabated, but so have the diseases, disabilities and deaths attributed to tobacco use, upped considerably. Clearly, enforcing the public health policies is an enormous challenge confronting India and other countries of the world.
Issues
According to the World Health Organization (WHO), tobacco is the only legal consumer product that can harm everyone exposed to it- and it kills up to half of those who use it . Yet, tobacco use is common throughout the world due to low prices, aggressive/ widespread marketing, lack of awareness about its dangers, and inconsistent public policies against its use. Most of tobacco’s damage to health does not become evident until years or even decades after the onset of its use. So, while tobacco use is rising globally, the epidemic of tobacco- related diseases and deaths has just begun.
The way forward
But we can change the future. The tobacco epidemic is devastating –but preventable. The fight against tobacco must be engaged forcefully and quickly- with no less urgency than battles against life-threatening infectious diseases. We can halt the tobacco epidemic and move towards a tobacco free world – but we must act now.
The Survey
Objectives
- To validate the national tobacco use statistics in India at Lucknow city level
- To find out the awareness level about existing key tobacco control policies in India
- To find out the community perceptions of the proven-cost-effective tobacco control interventions
- To disseminate the survey findings through different channels including media so as to inform the different stakeholders in tobacco control at national level.
METHOD
- Designing the questionnaire
o In a brainstorming session involving clinicians, researchers, statisticians, tobacco control advocates with substantial experience, we drafted the open-ended, unloaded, non-suggestive and objective questions in easy-to-read and understand Hindi language, so that respondents feel comfortable in opting for any given choice without any bias or prompt.
o The 15 questions (see annexure for the questionnaire) were broadly categorized in 4 categories:
- Personal information of respondents
- One section only for those respondents who were tobacco users on their tobacco use history
- One section to validate the key finding of the Bidi Monograph released by the Ministry of Health & Family Welfare, Government of India, in May 2008
- One section to evaluate the perceived effectiveness of key tobacco control policies and interventions being enforced in India.
o Every question had a set number of multiple choices which were coded (see questionnaire for data coding)- Data sheeto We used Microsoft Excel sheet and its formula to enter and analyze the data (see the data sheet attached in the annexure)
- Data collection
o We formed a team of data collectors or surveyors which included both men and women
o Lead surveyors were:
- Alok Kumar Dwivedi
- Sarika Tripathi
- Survey Briefing for surveyors
o Introduce yourself to the respondents and tell him/her about this survey.
o Take permission of the respondents before asking any question.
o Ask every question in an easy and informal manner so that respondents feel comfortable to opt for any given option without hesitation.
o Don’t react if a respondent is not responding to your question or feeling uncomfortable.
o Sample of respondents should not be biased towards a particular age group, educational status and/or sex .
o A respondent should be free to quit the survey any time.
o Show your questionnaire sheet to the respondents for their information.
- Data entry and analysis
o Data was entered by Alok Kumar Dwivedi and Sarika Tripathi as per the data coding and data entry excel sheet and formula-based software self-developed by them
o After data entry was completed, data was analyzed (see the output below) on different parameters
Survey Results
Out of the 763 respondents, 70 per cent were male and 30 per cent were female. According to a World Health Organization study of 2008, about 14.1% of the Indian teenagers are tobacco users---this percentage being 17.3 amongst males and 9.7 amongst females.

Tobacco consumption amongst adult males and females in India is respectively 57 per cent and 3.1 per cent. According to National Family Health Survey (NFHS), 2006, most tobacco users belong to the age group 18-24 years.
Maximum survey-respondents were in the age group of 30-50 years (44%), followed by the respondents in the age group of 18-30 years (39%). 11 per cent respondents were above 50 years of age and the least number of respondents were in the age group of 0-18 years (6%).
Age of respondents

Several data indicates that tobacco use is prevalent in people from different education backgrounds including those who don’t have any formal education. In this survey, most respondents were graduates (41%) followed by the remaining three categories without any significant difference: post-graduates (29%), undergraduates (28.10%) and those who had no formal education (31%).
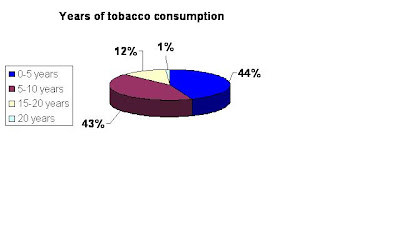
The survey data revealed that 57% of respondents had never consumed any form of tobacco, and 43% of the respondents were tobacco users. The survey data revealed that 44% of the respondents were using tobacco for the last 0-5 years, and 43% of the respondents were using tobacco for the last 5-10 years. 12% survey-respondents were using tobacco for last 15-20 years while 1% had consumed tobacco for 20 or more years.
Traditional forms of tobacco chewing such as paan now appear to be mainly an indulgence of the older generation; the younger generation is taking up newer forms of tobacco use such as, tobacco toothpaste, gutkha, and cigarette. Gutkha is a very common form of chewing tobacco. Our study revealed that 39 per cent of the respondents consumed gutkha, 32 per cent said that they smoked cigarette, 10 per cent of the respondents were bidi smokers, while 19 per cent of the respondents said that they had consumed all forms of tobacco products.
A World Health Organization (WHO) study reviewed 440 bollywood films released between 1991 and 2002 and, shockingly, found that tobacco consumption, mainly in the form of smoking, was shown in nearly three out of four movies. Tobacco use by the lead actors in movies can be directly related with youth’s initiation into smoking as a symbol of fashion and style. 36 per cent of the survey-respondents said that they began tobacco due to all the three factors that is stress, peer pressure and seeing film-actors smoking in movies. 30 per cent of the respondents said that they began using tobacco because of stress.
The results of the Global Youth Tobacco Survey, supported by the WHO and the Centres for Disease Control and Prevention (CDC), conducted in India during the years 2000-2004, revealed that over 68.5% of students who smoked wanted to stop whereas 71.4% had already tried to stop smoking during the past year. All over India, 84.6% of cigarette smoking students had received help or advice to stop smoking from family members, community members, health personnel or friends. In the survey conducted by us in Lucknow, the data also revealed that 69 per cent of the survey-respondents had attempted to quit tobacco use, while 31 per cent said that they had never tried to quit their tobacco habit.

The different forms of tobacco often do not include the same warning labels, taxes and other restrictions which are placed on cigarettes. Also gutkha, bidis and many other local forms of tobacco are manufactured and marketed in an unorganized sector to a considerable extent – making it further difficult to regulate these tobacco products. But is bidi more harmful or cigarettes? 49 percent of the survey-respondents were of the view that both cigarette and bidi are equally harmful while 30 percent said that bidi is more harmful than cigarette and 20 percent said that cigarette is more harmful than bidi. According to the bidi monograph released by the Ministry of Health and Family Welfare, Government of India in May 2008, bidis are, at least, as harmful as cigarettes.

Countries of comparable status to India, like Brazil, Thailand, Singapore, Hong Kong, Uruguay, Venezuela and a host of developed countries have devoted more than 50% of tobacco-pack space to picture-based tobacco warnings, many of them gorier than the proposed Indian pictures. The survey revealed that 52 per cent of the respondents felt that the pictorial warnings on tobacco packs will help raise awareness about tobacco-related hazards, while 45 per cent said that these pictorial tobacco warnings will have no effect in raising awareness. Since pictorial tobacco-warnings are yet to be implemented in India, these responses were based on, and reflect upon the perceptions and not actual field-testing data. Around the world, pictorial warnings on tobacco packs have significantly contributed to raise awareness, deter tobacco users and encourage them to quit tobacco use.

Pictorial warnings have proved to be highly effective in reducing the percentage of tobacco usage in countries like Canada, Australia, Belgium, Thailand, Brazil and the European Union where the tobacco usage has dropped, on an average, by 1% per annum post-implementation. The survey done in Lucknow also revealed that 37 per cent of the respondents felt that the pictorial tobacco warnings will encourage people to quit tobacco use, while 56 per cent said that pictorial warnings on tobacco packs will not motivate people to quit tobacco.

A WHO study revealed that the passive smoking is associated with ischemic heart disease (IHD), with a 30% excess risk of IHD in non-smokers whose spouses smoke compared with non-smokers whose spouses do not smoke. Non-smokers exposed to secondhand-smoke had a 25% excess risk of CHD (Coronary Heart Disease) compared to non-smokers not exposed to smoke in India. This survey revealed that an overwhelming majority of 73 per cent of the respondents wanted a complete ban on smoking in both public and private places.

A public interest litigation (PIL) was filed before the High Court of Kerala by a woman who complained of problems caused by exposure to tobacco smoke from co-passengers during frequent travel by bus. In response to this petition, the High Court delivered a judgment which stated that a public health law to eliminate exposure to second hand smoke is long overdue. The court held that the policy makers should pursue all the strategies that would help accomplish this goal. Upholding this judgment and recognizing the delay of the legislature in enacting a national law, the Supreme Court of India in November 2001 stepped in to ban smoking in public places such as schools, libraries, railway waiting rooms and public transport throughout the country. In a recent statement, Dr Anbumani Ramadoss, Union Health and Family Welfare minister, Government of India, said that from 2 October 2008 smoking will be completely banned in all public and private places. Regarding this declaration of Dr Ramadoss , 71 per cent of the survey-respondents felt that this ban will not be effectively implemented, and 19 per cent of the respondents felt that it could be implemented effectively.

Tobacco cessation services need to be scaled up drastically (and rapidly) to assist people to quit tobacco use successfully. This is going to complement other tobacco control interventions. This is also in line with the Framework Convention of Tobacco Control (FCTC). With the establishment of the National Tobacco Control Cell as part of the Government of India and World Health Organization (WHO) initiative on tobacco control in India, it was felt that tobacco cessation services have to be developed to help tobacco users in India give up their habit. In the survey conducted in Lucknow, 13% of the survey-respondents were aware of some proper tobacco cessation counsellng facility, while 57% of the survey-respondents weren’t aware of any such facility.

The Ministry of Health and Family Welfare, Government of India, has started Tobacco Cessation Clinics on a pilot basis in 13 centers. In 2002, the WHO supported the setting up of Tobacco Cessation Clinics (TCCs) in diverse settings (cancer treatment centers, psychiatric centers, medical colleges and non governmental organizations) to help people stop tobacco use. Lucknow’s Tobacco Cessation clinic was one such centre that WHO helped develop and expand.In the survey conducted in Lucknow, a stupendous majority of 96 per cent of the survey-respondents said that there should be a tobacco cessation clinic in all districts hospitals and primary health centres of the state. This clearly indicates the pressing demand for such tobacco cessation clinics, as perceived by the survey-respondents in the communities they come from.

Contacts:
Alok Kumar Dwivedi
Sarika Tripathi
Department of Public Health
Lucknow University



Comments
Post a Comment